Editor’s note: This article is part of a larger report, Healthcare’s $1 Trillion Challenge, which provides a roadmap for creating a more affordable and sustainable healthcare system. In this article, we offer solutions for generating $450 billion in savings over 10 years by reducing the administrative burden. Discover more chapters on lowering clinical labor costs and curbing the impact of growing drug costs.
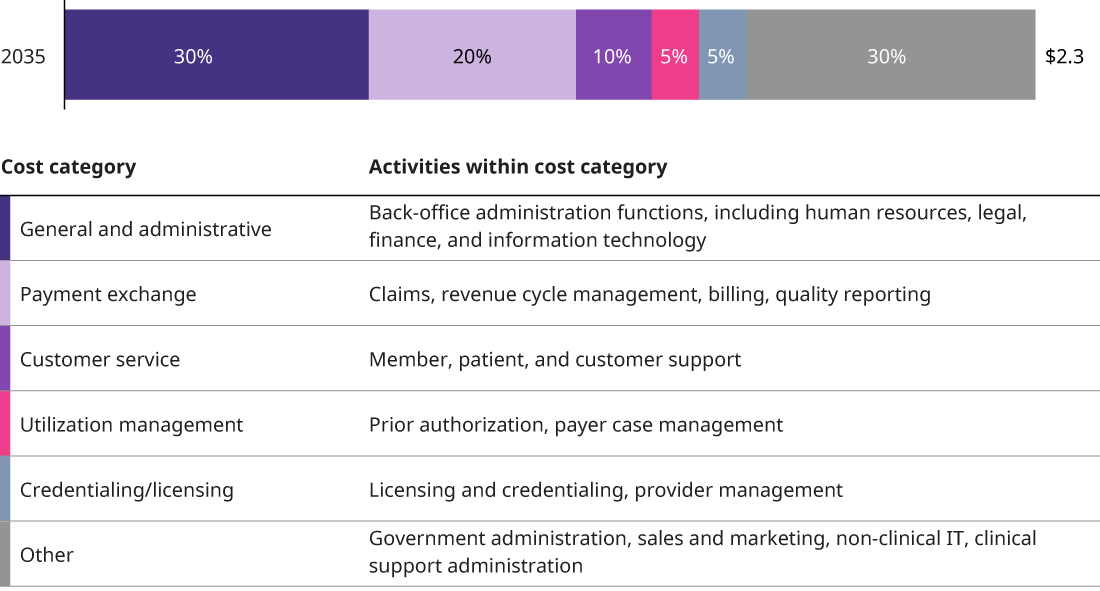
While administration functions in the US healthcare system are constrained by extensive regulation and a multi-payer structure, much of the work is ripe for efficiency reform. Studies conducted over the past two decades show that administrative costs have grown at the same rate as clinical spending, accounting for 25% of total health expenditures from 1999 through 2019. If trends continue, administrative costs will be $2.2 trillion in 2035, or $6,400 per capita.
This administrative burden is unsustainable and is starting to impact access to care. Nearly two-thirds of physicians cite administrative work as their top source of burnout. Non-clinical staff are also experiencing burnout at high rates, with some studies showing that 45% of non-clinical staff suffering from work overload and 32% expressing an intent to leave their job. The industry can achieve a more sustainable administrative cost base with more simplification, less fragmentation and unnecessary variation, improved technology systems, and better collaboration.
Reducing business costs in healthcare can save $125 billion
Functions nearly all businesses perform — human resources, legal, accounting – account for 40% of administrative costs. These are the costs of being in business, or general and administrative costs. Various studies, however, have shown that healthcare’s general and administrative expenses as a percent of revenues are nearly double those of other industries.
Back-office functions can benefit from best practices, new technology, and tools to improve workflows and cross-functional communication. For example, contract management remains a largely rudimentary and decentralized process for many payers. Yet there are plenty of contract management tools that digitize contract documents and allow for shared access and review. Some programs are implementing AI technology that can analyze contracts for inconsistencies and opportunities to renegotiate terms.
For providers, it is imperative to limit redundancies across administrative functions as systems consolidate and expand their care offerings and revenue streams. Investing in integration and change management programs to centralize functions from HR and legal to supply chain management and procurement will be essential to realizing cost and time efficiencies. Implementing modern software services that streamline planning and communication will further enhance efficiency outcomes. And automation can help health systems improve such tasks as staff scheduling and inventory management.
The industry can no longer afford to deprioritize opportunities to update basic corporate functions. Success here will require leaders to acknowledge this truth and invest time and money into process redesign and automation capabilities, as well as change management programs. Doing so could save the industry nearly 15% in the long term on back-office costs.
Four strategies to simplify healthcare processes and save $325 billion
The remaining 60% of costs are associated with processes that are more unique to healthcare. These activities occur along the entire care provision flow, from providing customer service and performing utilization management to submitting claims and managing provider information.
Many of these tasks are still conducted manually, like prior authorization submission and credentialing review. Processes like claims submission are not standardized. They are fragmented and plagued with complexity from high levels of variability across terms and policies. Misaligned perceptions of value from activities like utilization management frustrate payers and providers, resulting in duplicative and low-value work.
Simplifying these functions by leveraging smart technology, improving data management, and more effectively collaborating across stakeholders will relieve significant administrative burden — and cost — for payers and providers alike. For the four major administrative functions below, we have identified opportunities to simplify and reduce costs to achieve a more sustainable administrative cost base.
Improve customer and patient services via smart technology
Healthcare businesses employ an estimated quarter of a million people in the US alone answering phone calls from patients and members. By some counts, 84% of provider organizations still require appointments to be made via the front desk or a phone call, often to protect the schedules and preferences of individual physicians.
Enabling more self-service is a key to cutting spending on customer service activities. Automating and standardizing repeatable processes, such as appointment scheduling, check-in, and payment or benefits inquiries, will reduce resource needs for these activities. For example, expediting check-ins via patient portals or mobile apps is not only more convenient and less costly than in-office check-ins, but also more efficient for all parties involved.
Payer service to their provider partners is another area impeded by inefficiency. While a typical provider phone call on claims status or benefits verification can cost over $8 of the provider’s time, self-service is just cents on the dollar. Proactive measures, such as sharing claims status with provider partners via automated notification, can streamline communications. Leveraging large language capabilities in call centers, adding chatbots to websites, and using AI-supported computer-programmed platforms to respond to customer inquiries will increase efficiency and lower customer service labor costs.
Lastly, customer service teams should invest in improving technology platforms to streamline data management. Gathering customer information still requires customer service representatives to pivot between multiple screens and platforms. Modernizing supporting data structures will enable workflow efficiencies as well as reduce data inaccuracies.
Promote high-quality, high-value utilization management
Providers and payers can take steps to streamline how coverage and care decisions are made. While utilization management has long been a point of friction, there are meaningful opportunities to create a more efficient system that reduces costs and improves health outcomes.
One way to reduce costs is to improve the quality of prior authorization submissions. Providers will produce more accurate submissions when rules and requirements for clinical documentation are standardized and clearly documented. Tools that integrate electronic health record systems and submission portals will also enhance quality and efficiency by enabling direct document submission and automated data population. Payer-provider data connectivity is further encouraged by interoperability standards requiring the use of application programming interfaces that hasten data transfer and allow direct payer access to providers’ EHR systems. It is also time, at long last, to say goodbye to the fax machine. Despite significant cost savings opportunities, less than one-third of prior authorization was conducted electronically in 2022. Easy-to-use portals will promote digital prior authorization submission and reduce paper submissions, which take significantly more time to process.
On the payer side, prior authorization review procedures can be enhanced with machine learning, AI, and other smart technology tools. There is already motivation for payers to reform these practices. New CMS rules taking effect in 2026 require payers to adhere to short decision turnarounds, provide a reason for denials, and publicly report certain prior authorization metrics. Implementing auto-approval and AI-assisted review tools that pre-scan clinicals, summarize submissions, highlight spots requiring manual review, and provide a likelihood of approval score will speed up review times and minimize manual screening loads.
Lastly, there has already been material progress in reducing low-value prior authorization. Payers are increasingly removing or easing requirements in cases where care pathways are clearly defined. More creative solutions to limit prior authorization are also gaining popularity. For example, new risk programs remove all utilization management for a specific care pathway when providers assume financial risk for the care. Payers are also automatically removing prior authorization requirements if care is provided in a more optimal site of care such as the home or at the payer’s preferred site. Encouraging such programs has the potential to significantly reduce administrative burdens, while maintaining levels of care quality.
Reduce complexity in the claims and payment process
In 2035, payers and providers will spend nearly half a trillion dollars on submitting, reviewing, and paying claims. This is largely driven by the cost to maintain the inherent complexity of the system. Adhering to the dizzying array of benefit structures, payment models, carve-outs, and contract rules strains payers and providers along the entire claims and payment process. Digital systems for compiling and reviewing claims are not built to handle high levels of customization, which in turn requires expensive and time-consuming manual intervention. In efforts to minimize operational costs, payers and providers invest in vendors and AI technology to handle complex cases and negotiation — ultimately contributing to a high-cost arms race that adds even more administration.
While regulation that minimizes low-value variation across organizations is necessary to relieve significant burden, individual players can make changes now to meaningfully reduce spending while maintaining some optionality.
It is important that claim submissions are accurate and complete. Providers and payers can work together to implement new tools and processes that improve claims quality and reduce manual effort. Such tools include automated data entry and patient coverage verification embedded in EHRs, and AI-powered submission guidance, including rule clarification, preliminary reviews for missing or incorrect information, and next-steps guidance. Building these capabilities requires significant shared investment from payer-provider partners. Organizations will need to work together to construct robust data exchange processes allowing on-demand sharing of accurate patient, provider, and contract data. These investments will not only improve the quality of claims, but ultimately reduce individual spend on handling errors down the line.
Streamlining credentialing and licensing to support healthcare growth
The fragmented and intensive credentialing and licensing process is another pain point within administrative tasks. After compiling an application, physicians often spend over five months waiting to be credentialed with a payer or licensed in another state. And payers must sift through multiple applications submitted in various formats. Many of these processes are outsourced today, which makes savings within the current operational structure limited, but payers should continue to seek opportunities to digitize and outsource the submission and review process.
Relatedly, payers should invest in comprehensive provider data management systems to track and manage information. Each time a physician is newly credentialed, or changes their hours or practice location, payers must make updates, usually manually, across their various databases. Building tools that allow for automatic intake and real-time updates of provider information will save time and improve data accuracy. Upgrades to these systems will become even more critical as non-physician professionals are empowered to practice to the top of their license.
Optimizing administrative processes within the existing structures of the industry can save the healthcare industry $450 billion. All these levers require upfront investment in order to realize downstream savings. Many of them require collaboration across payers, providers, and vendors to improve overall process quality. And the healthcare industry has historically had an up-and-down relationship with new technology — there have been cases where technological updates have improved data capture or patient experience at the cost of productivity. But relying on outdated, broken processes is not a solution. Stakeholders need to shift from short-term reacting to long-term planning and make the case for meaningful investment to upgrade the foundational processes that enable healthcare delivery.
Removing structural barriers to unlock healthcare cost savings
Of all the cost drivers in healthcare, administration has one of the highest potentials for disruption. But that requires industry and regulatory actors to partner on mandatory structural changes and seize the opportunity for widespread standardization and simplification across administrative functions.
Significant value in the claims and payment process can be unlocked with government-backed standardization requirements. For example, CMS could drive more standardization in diagnoses that can and cannot be combined with certain procedures or implement a uniform coding system. These actions would reduce claim complexity and allow payers and providers to save time and investment on tools that streamline handling of complex claims.
Another concept that’s been discussed before in healthcare administration reform borrows from the banking industry: a centralized payment clearinghouse. Today, a single healthcare claim will often travel through multiple clearinghouses to match and compare billing information. A single centralized claims clearinghouse would enforce the standardized exchange of billing information, effectively eliminating the low-value variations involved today.
Streamlining quality reporting is another area that is ripe for reform. Providers spend considerable time preparing and reporting quality data for stakeholders, each with different reporting requirements. One study pegged it at over 100,000 person-hours for one hospital. A mandated set of metrics, and restrictions on the ability to add additional bespoke metrics could radically simplify this process.
Standardization could also reduce the burden of utilization management. This includes creating uniform care pathway definitions for common cases, likely through collaborative efforts between the federal government and independent agencies, and enforcing gold carding programs, which allow providers who meet certain criteria to be exempted from an insurer’s prior authorization or receive a streamlined process. In response to a perceived overload of requirements, certain states have already enacted laws requiring various forms of gold carding. Individual payers have also introduced programs to slim down prior authorization requirements. And national reform such as the so-called GOLD CARD Act, which would exempt qualifying physicians from certain prior authorization requirements under Medicare Advantage plans, was introduced to Congress in 2023.
The value of standardization also extends to physician licensing and credentialing, where a nationally regulated process would enable physicians to seamlessly practice across states and limit time spent on compiling applications. Centralizing provider information in a federally supported central site would minimize time and effort spent on credentialing physicians for all payers.
A simplified administrative model to reduce healthcare costs by 2035
In 2035, the number of people working in administration will be considerably lower than today, for both providers and payers. As cost pressures increase, payers and particularly providers who achieve and maintain lean administration will be increasingly rewarded and outcompete the market. The industry will bend the cost curve, so that administrative costs no longer keep pace with clinical costs and begin to realize economies of scale.
